Prurigo Nodularis
An Introduction to Prurigo nodularis
Prurigo nodularis (PN) is a chronic inflammatory skin disease with pruritic nodules. PN lesions may occur in any age group but are most commonly seen in older adults. It can be associated with another cutaneous hypersensitivity disorder, such as atopic dermatitis or chronic pruritus, and its exact aetiology remains poorly understood. The condition is associated with significant physical and psychological morbidity and is often refractory to treatment. With currently limited agents approved by the US Food and Drug Administration, the management of PN is difficult, and available treatment options are often multimodal due to the intersection of neuroimmune etiologic factors in the pathogenesis of PN. Novel therapies such as monoclonal antibodies, opioid-antagonists and interleukin-31 targeting agents are emerging, providing hope for this patient population.

Physician burnout is at a critical point. In this episode, Nicky speaks with Dr Alfred Atanda about why so many physicians are burning out and what can be done to change the trend. From personal experience to system-wide solutions, Dr Atanda shares valuable insights on improving physician well-being and building a more effective healthcare culture.
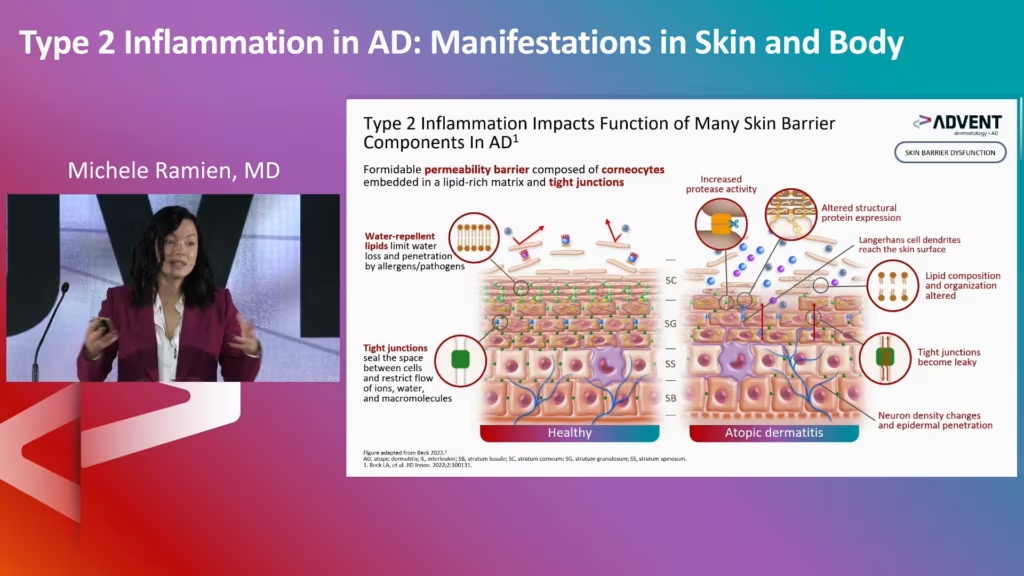
Watch leading experts discuss the pathophysiology of AD, PN, and CSU, and the concepts of AD remission and disease modification.

The FDA has approved nemolizumab-ilto (Nemluvio; Galderma) for treating prurigo nodularis, a chronic skin condition characterized by intensely itchy nodules. Nemolizumab is the first approved monoclonal antibody specifically inhibiting the signaling of IL-31, a neuroimmune cytokine that drives multiple disease mechanisms in prurigo nodularis

Recent advancements made in understanding the pathology of inflammatory skin conditions have enabled JAK inhibitors, initially developed for haematology over 20 years ago, to be investigated for dermatological use. In this episode, Dr William (Bill) Damsky discusses JAK inhibitors’ journey from proof-of-concept to treating a wide range of skin conditions, their future impact on rare diseases and the debate around safety.
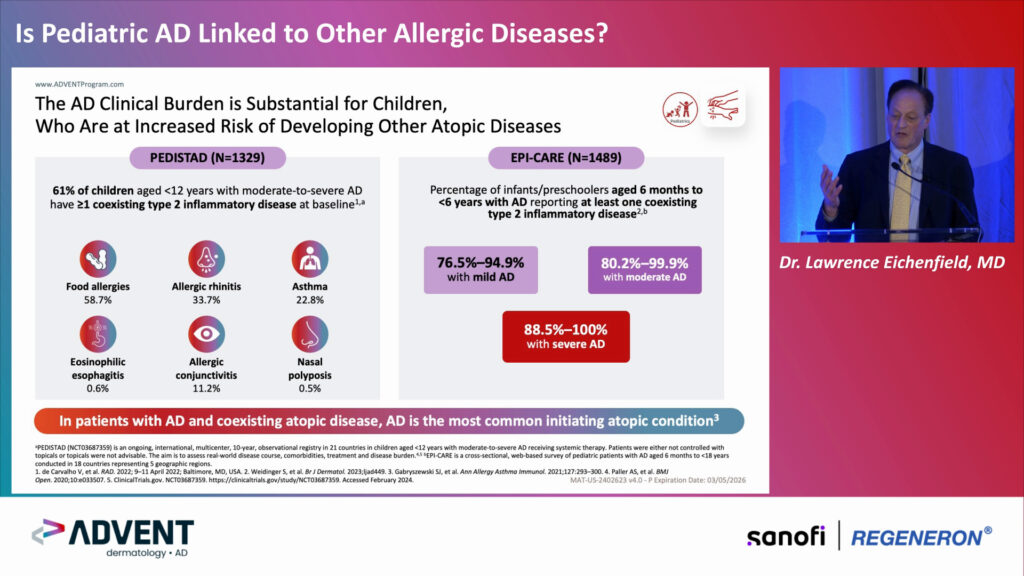
Watch highlights of two ADVENT symposia originally presented in San Diego, March 2024.

Select a discussion in our hub to watch our multidisciplinary experts, including a patient advocate, share important perspectives on the need to establish patient-centric treatment and care pathways for the management of prurigo nodularis.









OLYMPIA 2 (NCT04501679) was a phase 3, multicentre, double-blind study that investigated the IL-31 inhibitor nemolizumab for the treatment of prurigo nodularis in adults. touchDERMATOLOGY were delighted to speak with Prof. Adam Reich (University of Medicine, Wroclaw, Poland) around his analysis of OLYMPIA 2, looking at improvements in pain and patient reported outcomes. The abstract ‘Nemolizumab modulates prurigo nodularis-associated skin pain and markedly improves patient reported outcomes in patients with moderate-to-severe prurigo nodularis in a phase 3 study (OLYMPIA 2).' (Abstract N°: 4147) was presented at EADV 2023, Berlin, 11-14 October 2023 #EADVCongress. Questions What is the mechanism of action and rationale for investigating nemolizumab in prurigo nodularis? (0:18) Could you describe the aims and design of the phase 3 OLYMPIA 2 study, and how well the key endpoints were met? (0:50) What additional outcomes were investigated in your analysis of OLYMPIA 2 and how well were they met? (1:29) What will be the next steps in the clinical development of nemolizumab? (2:05) Disclosures: Adam Reich discloses receiving grant/research support from Abbvie, Anaptys, BMS, Dice, Eli Lilly, Galderma, Incyte, Jannsen, Medac, Novartis, Pfizer, Regeneron, Trevi Therapeutics, and UCB; serving on advisory boards for Abbvie, Galderma, Leo Pharma, Sanofi, Novartis, and Eli Lilly. Support: Interview and filming supported by Touch Medical Media Ltd. Interview conducted by Victoria Jones and Katey Gabrysch. Filmed in coverage of the EADV Annual Meeting. This content was developed by Touch Medical Media and is not affiliated with the European Academy of Dermatology & Venereology (EADV) or the congress.

Atopic dermatitis and prurigo nodularis are type 2 inflammatory skin diseases with intense pruritis. Both share mechanisms of disease, including inflammation with the role of type 2 cytokines in driving itch. We were delighted to speak to Expert Faculty member Dr. Raj Chovatiya (Northwestern University Feinberg School of Medicine, Chicago, IL, USA) to discuss the burden of itch and its impact on quality of life, dupilumab’s recent approval and its impact on the treatment landscape. Questions Could you describe the burden of itch and the impact this has on patient quality of life? (0:17) What impact has the approval of dupilumab had on the treatment paradigm for pruritic diseases? (0:56) How do atopic dermatitis (AD) and prurigo nodularis (PN) differ in presentation, despite sharing a similar pathology? (1:29) Aside from relieving itch, what other benefits are associated with targeting IL-4 and IL-13 signalling in AD and PN? (2:13) What are the next steps to achieving disease control in inflammatory skin diseases? (2:42) Disclosures: Raj Chovatiya discloses advising, consulting, and/or speaking for AbbVie, Apogee Therapeutics, Arcutis, Argenx, ASLAN Pharmaceuticals, Beiersdorf, Boehringer Ingelheim, Bristol Myers Squibb, Cara Therapeutics, Dermavant, Eli Lilly and Company, FIDE, Galderma, Genentech, GSK, Incyte, Janssen, LEO Pharma, L’Oréal, Nektar Therapeutics, Opsidio, Pfizer Inc., Regeneron, RAPT, Sanofi, and UCB. Support: Interview and filming supported by Touch Medical Media Ltd. Interview conducted by Victoria Jones and Katey Gabrysch. Filmed in coverage of the EADV Annual Meeting. This content was developed by Touch Medical Media and is not affiliated with the European Academy of Dermatology & Venereology (EADV) or the congress.

LIBERTY-PN PRIME (NCT04183335) was a randomised, double-blind, placebo-controlled phase 3 trial, investigating dupilumab for the treatment of prurigo nodularis. touchIMMUNOLOGY caught up with Prof. Gil Yosipovitch (Miller School of Medicine, University of Miami, Miami, FL, USA) to discuss the aims, design ...
Watch three experts discuss the symptom burden faced by patients with prurigo nodularis, and how clinicians can optimize diagnosis and treatment of the disease.
Latest articles videos and clinical updates - straight to your inbox
Log into your Touch Account
Earn and track your CME credits on the go, save articles for later, and follow the latest congress coverage.
Register now for FREE Access
Register for free to hear about the latest expert-led education, peer-reviewed articles, conference highlights, and innovative CME activities.
Sign up with an Email
Or use a Social Account.
This Functionality is for
Members Only
Explore the latest in medical education and stay current in your field. Create a free account to track your learning.

