Introducing the touchDERMATOLOGY Future Leaders 2025
This year, we are celebrating our inaugural touchDERMATOLOGY Future Leaders to recognize the outstanding talent that has entered our field in recent years. These individuals are set to innovate and transform dermatology in the years to come.
3 Questions with Neelam Vashi: touchDERMATOLOGY Future Leader 2025
We are delighted to introduce touchDERMATOLOGY Future Leader, Dr Neelam Vashi, a highly accomplished dermatologist widely recognized for her expertise in cosmetic dermatology, skin of colour and laser medicine.
What roflumilast 0.3% foam brings to your psoriasis clinical toolkit
To better understand how this newly approved therapy fits into clinical practice, what the data show and which patients are likely to benefit, we spoke with Dr Jennifer Soung
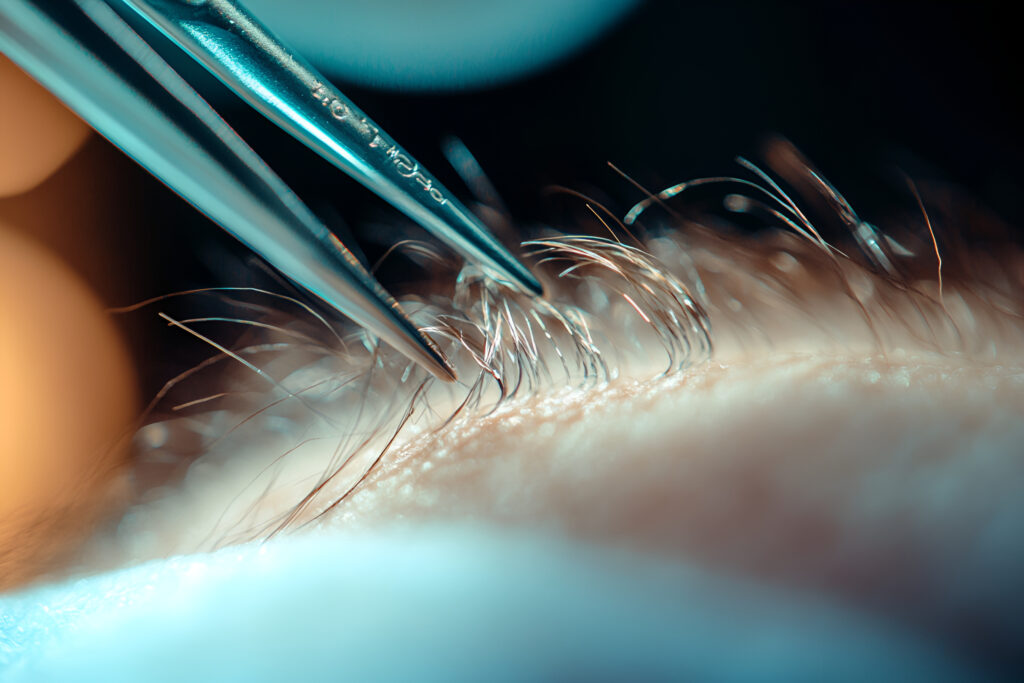
Polish up: What’s new in diagnosing and treating onychomycosis
Onychomycosis is one of the most common nail conditions seen in clinical practice, yet diagnosis is often uncertain and treatment failures are frustratingly common. In this episode, Dr Shari Lipner shares practical updates on smarter diagnostics, existing & emerging therapies, and what we need to know about how to manage this condition today and in the future.
01. Introducing the touchDERMATOLOGY Future Leaders 2025
02. 3 Questions with Neelam Vashi: touchDERMATOLOGY Future Leader 2025
03. What roflumilast 0.3% foam brings to your psoriasis clinical toolkit
04. Polish up: What’s new in diagnosing and treating onychomycosis
Onychomycosis is one of the most common nail conditions seen in clinical practice, yet diagnosis is often uncertain and treatment failures are frustratingly common. In this episode, Dr Shari Lipner shares practical updates on smarter diagnostics, existing & emerging therapies, and what we need to know about how to manage this condition today and in the future.

The FDA recently approved roflumilast 0.3% foam for the treatment of plaque psoriasis of the scalp and body in both adolescents and adults. To better understand how this newly approved therapy fits into clinical practice, what the data show and which patients are likely to benefit, we spoke with Dr Jennifer Soung (Harbor University of California, Los Angeles and Southern California Dermatology, Santa Ana, CA, USA), a key investigator on the phase 3 ARRECTOR trial.

Physician burnout is at a critical point. In this episode, Nicky speaks with Dr Alfred Atanda about why so many physicians are burning out and what can be done to change the trend. From personal experience to system-wide solutions, Dr Atanda shares valuable insights on improving physician well-being and building a more effective healthcare culture.
Could targeting hair follicle stem cells be the key to reversing, and even preventing, age-related hair loss? In this episode, we’re joined by Dr Jon Edelson to explore a novel approach that could address the root cause of age-related hair loss. With no new approved treatments in decades, this cutting-edge strategy could represent a major leap forward. Tune in as we discuss the science behind stem cell reactivation and how it could reshape the future of hair restoration for the millions of men and women affected by this form of hair loss.

The International Society of Dermatology (ISD) stands at the forefront of advancing global skin health through education, collaboration and outreach.1 Established with a mission to bridge disparities in dermatological care worldwide, the ISD has become a vital hub for connecting ...
Pyoderma gangrenosum (PG) is a rare, painful and complex autoimmune skin condition that can present significant diagnostic and treatment challenges.1 To provide expert insights into this challenging disease, we spoke with Dr Benjamin Kaffenberger, a dermatologist at The Ohio State ...
With a career that spans continents, Prof. Dedee Murrell stands out as a global leader in dermatology and a passionate advocate for women in medicine. In this episode, we sit down together to explore her inspiring journey—from her early years in the UK and medical training in the USA to pioneering therapies for some of dermatology’s rarest and underserved conditions in Australia. We also reflect on her recent MDS Lifetime Achievement Award and discuss the value of mentorship, strategies for advancing a career in dermatology and academic medicine, and how to stay at the cutting edge of medical innovation.

Renowned for his work in urticaria, drug allergies and angioedema, Professor Luis FC Ensina is a distinguished allergologist. As a Professor of the Division of Allergy, Clinical Immunology and Rheumatology at the Federal University of São Paulo, Brazil and ...
touchDERMATOLOGY coverage from EADV 2024: Twice-daily continuous application of ruxolitinib cream, a topical selective JAK1/JAK2 inhibitor, has been reported to be safe and effective in treating children with mild to moderate atopic dermatitis (AD) over an 8-week period in the ...

Dr. Shari Lipner is a leading expert in dermatology, best known for her specialization in nail disorders. As an Associate Professor of Clinical Dermatology and Director of the Nail Division at New York-Presbyterian/Weill Cornell Medical Center, her work bridges ...

Recent advancements made in understanding the pathology of inflammatory skin conditions have enabled JAK inhibitors, initially developed for haematology over 20 years ago, to be investigated for dermatological use. In this episode, Dr William (Bill) Damsky discusses JAK inhibitors’ journey from proof-of-concept to treating a wide range of skin conditions, their future impact on rare diseases and the debate around safety.
In this episode, we explore the future of continuing medical education (CME) with the team behind touchIME. Hannah Fisher and Matthew Goodwin share insights into global and US trends, the importance of patient inclusivity and how educational outcomes are evolving to better measure the direct impact of learning on clinical practice and patient care.

Janus kinase inhibitors (JAKis) have transformed the landscape of dermatological therapy over the last 2 years, with six United States Food and Drug Administration approvals and further clinical trials in progress.1 JAKis have proven highly efficacious in dermatological diseases, by blocking ...

Chronic spontaneous urticaria (CSU), a common and distressing skin condition driven by mast cells, is typically managed with a stepwise approach using second-generation H1-antihistamines, omalizumab and cyclosporine, as recommended by international guidelines. However, many patients with CSU do not ...

The pathogenesis of cutaneous granulomatous disorders is incompletely understood and many unmet needs remain in the treatment paradigm.1 These disorders can be categorized into two main groups: those caused by infections and those associated with inflammatory skin conditions, among the ...
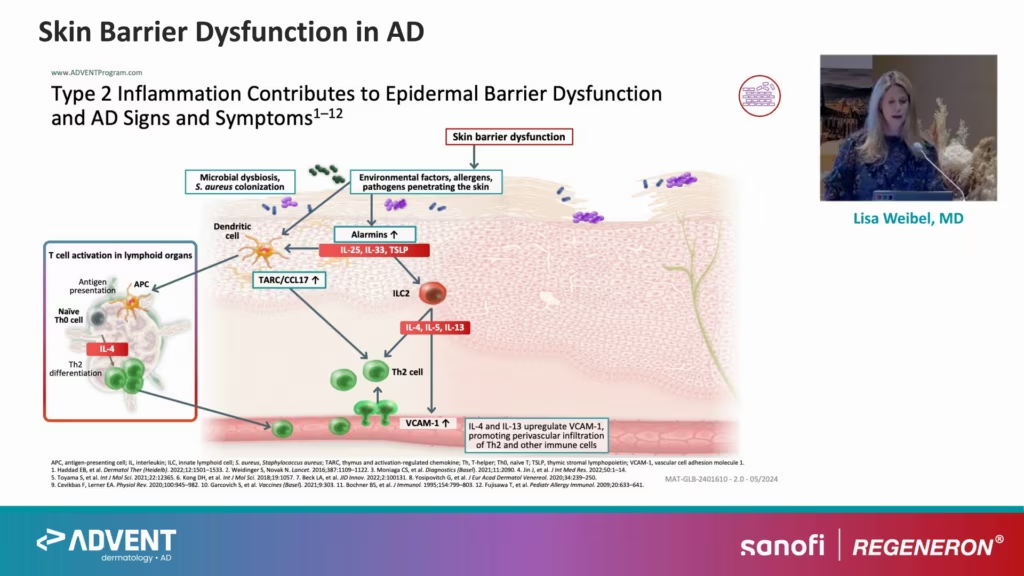
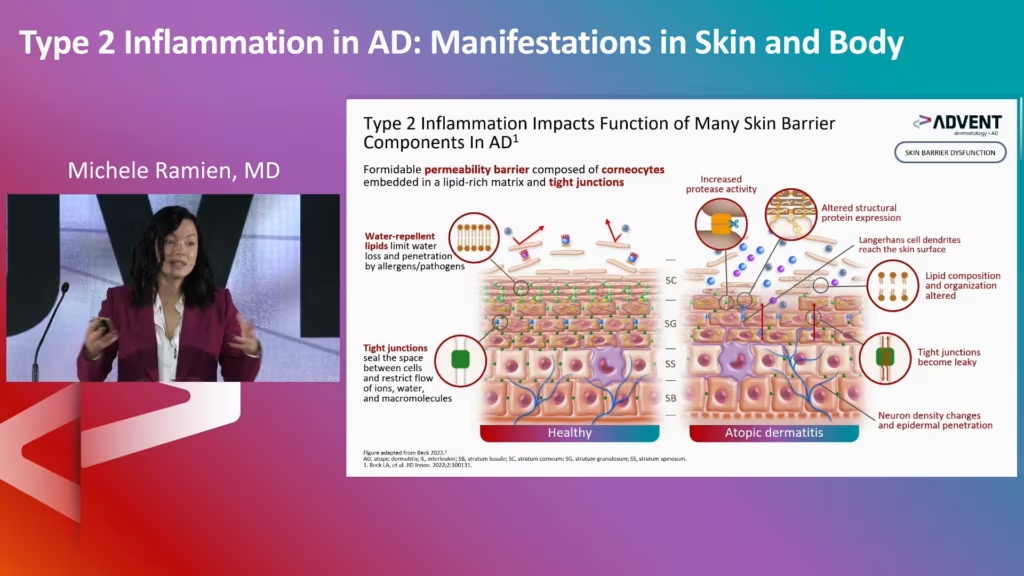
ADVENT at ESPD 2024: Type 2 Inflammation in Atopic Dermatitis and the Benefits of Early Intervention
Join experts Lisa Weibel, Amy Paller, and Eulàlia Baselga as they investigate the inflammatory processes driven by type 2 cytokines that lead to the local and systemic clinical effects of AD.
Watch leading experts discuss the pathophysiology of AD, PN, and CSU, and the concepts of AD remission and disease modification.

Watch leading experts discuss updates in the treatment of chronic spontaneous urticaria (CSU), based on data presented at EAACI 2024.
Editorial Board
Introducing the Expert Faculty of touchDERMATOLOGY, who support our mission to advance medical knowledge and practice by ensuring the integrity, relevance, and impact of the content we publish. Together, we strive to foster a vibrant academic community and contribute to the continuous improvement of healthcare worldwide.

Dedee Murrell
Faculty member
Blistering Diseases

Dedee Murrell
Faculty member
Professor and Head of Department of Dermatology, St George Hospital, University of NSW, Australia
Biography
Professor Dedee Murrell completed medical training at Cambridge and Oxford Universities, 3 years of internal medicine in the UK and USA, dermatology training at UNC-Chapel Hill, a fellowship in dermatopharmacology at Duke, blistering diseases and cell biology at New York University, and then became a clinical scholar at Rockefeller University. She holds a doctorate on the pathogenesis of blistering disorders, her main subspecialty interest, and her current research focusses on the development and validation of clinical outcome measures for autoimmune blistering diseases and epidermolysis bullosa to enable clinical trials to proceed in these orphan diseases. She has 418 peer reviewed papers, 16,7500 citations, an H index of 61, i!) of 213 and has edited 6 books, including the textbook, Blistering Diseases. She lectures at international congresses regularly and is a visiting professor in 5 continents. She was Congress President of the ICD 2021, the world’s first virtual Dermathon. She was founding Co-Editor of the International Journal of Women’s Dermatology and serves on the editorial boards of BJD, JAMA Dermatology, International Journal of Dermatology, JEADV, Acta Dermatovenereologica and JAAD International. She established Australia’s first dedicated dermatology clinical trial centre and is a KOL in trial design and conduct, serving on numerous advisory boards for more than 20 years. Her group established the ABQOL/TABQOL for measuring QOL in AIBD and she co-led the development and validation of the PDAI, BPDAI and MMPDAI. She established the Australasian Blistering Diseases Foundation in 2006.

William Damsky
Faculty member

William Damsky
Faculty member
Dermatological disorders

William Damsky
Faculty member
Assistant Professor of Dermatology at Yale School of Medicine, New Haven, CT, USA
Biography
William Damsky, MD, PhD is an Assistant Professor of Dermatology at Yale School of Medicine and board-certified dermatologist and dematopathologist. In clinical practice, he specializes in evaluation and treatment of patients with inflammatory skin disorders, especially cutaneous granulomatous diseases such as sarcoidosis and granuloma annulare. Dr. Damsky is interested in the identification and evaluation of new treatment approaches for inflammatory skin disease and conducts clinical trials in this area. As a physician-scientist with training in basic immunology, Dr. Damsky’s laboratory leverages the latest immunologic approaches to understand mechanisms of inflammatory skin disease and how they are affected by novel therapies. Dr. Damsky’s research has been supported by Career Development Awards from the Dermatology Foundation and the National Institute of Allergy and Infectious Diseases (NIAID). He was awarded the 2020 Young Investigator Award by the American Academy of Dermatology for his research in novel therapeutics for sarcoidosis.
Dedee Murrell
Faculty member


Raj Chovatiya
Faculty member

Raj Chovatiya
Faculty member
Atopic Dermatitis

Raj Chovatiya
Faculty member
Clinical Associate Professor, Rosalind Franklin University Chicago Medical School; and Founder and Director, Center for Medical Dermatology and Immunology Research, Chicago, IL, USA
Biography
Raj Chovatiya, MD, PhD, MSCI is Clinical Associate Professor of Medicine at Rosalind Franklin University Chicago Medical School and Founder and Director of the Center for Medical Dermatology + Immunology Research in Chicago, Illinois. His clinical and research focus includes the intersection of cutaneous immunology and inflammatory disease. He received his MD and PhD in immunology from Yale and completed his residency, postdoctoral research fellowship, and MS in Clinical Investigation at Northwestern University where he also served as Chief Resident. Dr. Chovatiya has a particular interest in optimizing patient-centered care, understanding chronic disease burden especially in understudied inflammatory diseases, exploring health and social disparities, and improving care across diverse skin types. He has published numerous abstracts and manuscripts and has been nationally and internationally recognized for his contributions as a clinician, educator, researcher, and leader.
William Damsky
Faculty member


David Rosmarin
Faculty member

David Rosmarin
Faculty member
Psoriasis and Atopic Dermatitis

David Rosmarin
Faculty member
Chair of the Department of Dermatology at Indiana University
Biography
Dr. David Rosmarin is the Chair of the Department of Dermatology at Indiana University and a clinical investigator. He previously served as Vice-Chair for Research and Education at Tufts Medical Center focusing on clinical trials for inflammatory disorders of the skin. For his training, Dr. Rosmarin went to medical school at NYU, dermatology residency at Boston University-Tufts Combined training program, and fellowship at Brigham and Women’s Hospital. Dr. Rosmarin joined Tufts Medical Center in 2013 focusing as a clinical trial investigator. In 2016, Dr. Rosmarin became the Director of the Clinical Trials Unit in the Department of Dermatology at Tufts Medical Center. Dr. Rosmarin’s studies have resulted in him becoming the PI for multicentered trials evaluating topical ruxolitinib in vitiligo, which has led to the first ever FDA indication for repigmenting vitiligo. Dr. Rosmarin is the first to use dupilumab for bullous pemphigoid which is now in a phase 3 program for an indication. Clinically Dr. Rosmarin is nationally recognized and serves as a referral for physicians with difficult to manage inflammatory diseases such as atopic dermatitis. Dr. Rosmarin educates medical students, residents, and research fellows. He served as Residency Program Director from 2016 to 2020 in which time he expanded the Tufts Medical Residency Program from nine positions to twelve residents and mentors faculty in education and research.
Raj Chovatiya
Faculty member


Dedee Murrell
Faculty member

 touchDERMATOLOGY
touchDERMATOLOGY
Register Now!
Explore the latest in medical education and stay current in your field. Create a free account to track your learning.
- Save your progress for video
- Keep track of your CME credits
- Add personalised learning notes
- Receive updates from course leaders and faculty
- Be the first to hear about new and exciting interactive learning opportunities
Latest articles videos and clinical updates - straight to your inbox
Log into your Touch Account
Earn and track your CME credits on the go, save articles for later, and follow the latest congress coverage.
Register now for FREE Access
Register for free to hear about the latest expert-led education, peer-reviewed articles, conference highlights, and innovative CME activities.
Sign up with an Email
Or use a Social Account.
This Functionality is for
Members Only
Explore the latest in medical education and stay current in your field. Create a free account to track your learning.