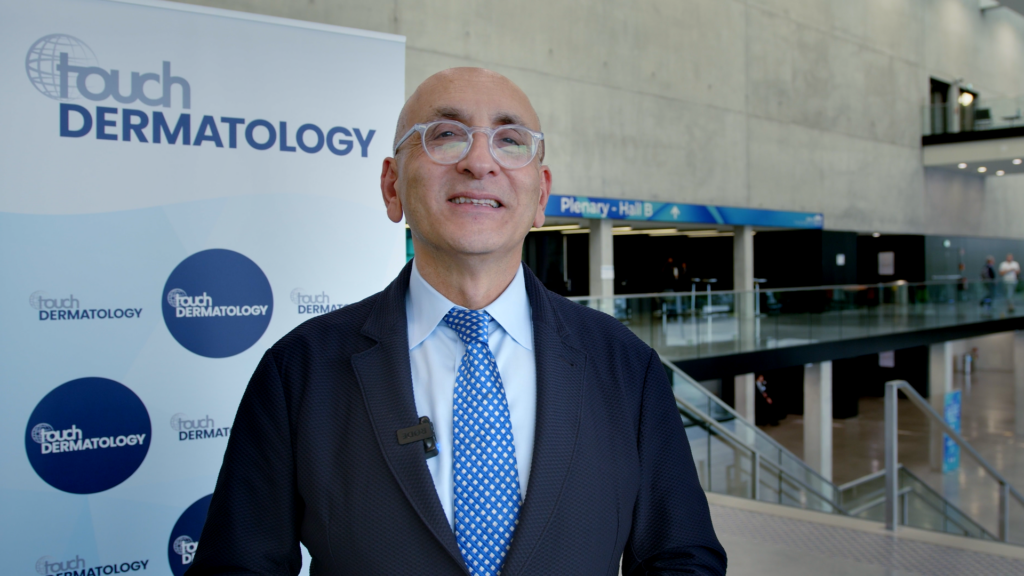
Touch Medical Media coverage of data presented at EADV 2023:
GUIDE is a phase 3b randomized, parallel-group, double-blind trial investigating guselkumab for the treatment of moderate-to-severe psoriasis (NCT03818035). We were delighted to speak with Prof. Knut Schäkel (University Hospital Heidelberg, Germany) to discuss the clinical data already supporting GUS from GUIDE 1 and 2, and the rationale, methodology and findings from GUIDE part 3, which were presented at EADV.
The abstract ‘Treatment-free period of more than 1 year in guselkumab super responders with short disease duration of psoriasis: withdrawal data from the GUIDE trial‘ (Abstract N°: 2042) was presented at EADV 2023, Berlin, 11-14 October 2023 #EADVCongress.
Questions
- What were the aims, design and eligibility criteria of the Phase 3b GUIDE trial? (0:16)
- What data from GUIDE 1 and 2 already supports early intervention with GUS? (1:28)
- Could you describe the rationale and methodology of GUIDE part 3? (2:19)
- What were the clinical endpoints and how well were these achieved? (3:10)
- What significance do these findings have in terms of maintenance of response following GUS withdrawal? (4:06)
Disclosures: Knut Schäkel has been an advisor and/ or received speakers’ honoraria and/ or received grants and/ or participated in clinical trials of the following companies: AbbVie, Almirall, Antabio, Boehringer Ingelheim, Celgene, Eli Lily, Galderma, Janssen-Cilag GmbH, LEO Pharma, Novartis, Pfizer and UCB Pharma.
Support: Interview and filming supported by Touch Medical Media Ltd. Interview conducted by Victoria Jones and Katey Gabrysch.
Filmed in coverage of the EADV Annual Meeting.
This content was developed by Touch Medical Media and is not affiliated with the European Academy of Dermatology & Venereology (EADV) or the congress.
Click here for more content on psoriasis & for further EADV 2023 highlights visit here.
Transcript
My name is Prof. Knut Schäkel. I’m an Assistant Director of Dermatology at the University Clinic in Heidelberg, Germany.
What were the aims, design and eligibility criteria of the Phase 3b GUIDE trial? (0:16)
We know that with modern biologics, we can treat psoriasis patients effectively. However, we aimed to go a step further to see if we could influence the immune system more significantly—hence, the GUIDE study was designed. Forty percent of the participants had a disease duration of two years or less, and we wanted to observe their response to the treatment. In part two of the study, they received treatment every eight or every sixteen weeks.
The primary endpoint was to assess their condition after 68 weeks post-treatment cessation. This study is intriguing not only clinically but also because of the biomarker data we collected through biopsies and blood samples, which should provide deeper insight into the biology at play.
What data from GUIDE 1 and 2 already supports early intervention with GUS? (1:28)
In the first phase, we aimed to identify ‘super responders’—patients who, by week 20 and week 28, were completely free of any disease. We explored whether these were individuals with a shorter or longer disease duration. It emerged that 43% of patients with a shorter disease history became super responders, while 27% of those with a longer history also responded well. This was a significant finding, showing a clear advantage for patients diagnosed more recently.
Could you describe the rationale and methodology of GUIDE part 3? (2:19)
The subsequent question was how long this strong treatment response could be preserved. Previous studies indicated that after one year, some patients still exhibited a PASI 90, particularly those with a shorter disease duration. This observation led to a more targeted approach.
What were the clinical endpoints and how well were these achieved? (3:10)
At week 68, patients were taken off the drug, and we’ve been monitoring them closely. Our interim analysis at 116 weeks—when patients had been off treatment for over a year—was quite revealing.
The primary clinical endpoint was whether super responders could maintain their condition with treatment every 16 weeks instead of the standard 8. This was a crucial consideration, especially when patients need to interrupt treatment for other health issues. The results confirmed that there was no difference in efficacy between the two dosing schedules among super responders.
What significance do these findings have in terms of maintenance of response following GUS withdrawal? (4:06)
We can assert that patients with a shorter duration of psoriasis respond better. They not only tolerate less frequent dosing but also maintain their improved condition after drug withdrawal. After thirteen months, 27% of these patients still had a PASI less than five. This indicates a prolonged response, particularly in those diagnosed more recently, and leads us to hope that we might be observing a change in the immune system—a potential move towards disease modification.
So if you treat early, you reach a stronger response and maybe you can also change the immune response.